Using values-based communications to improve patient response
By Tyler Wilson, VP of Population Health and Clinical Quality, Austin Regional Clinic
Austin Regional Clinic, in conjunction with health consulting firm MDH Consulting, has been working to improve communications with patients on specific messages, with the end goal of engaging more patients to keep up with their preventive health care screenings and the management of their chronic diseases. In this case, we have categorized patients based on their attitude and response to healthcare communications and then crafted specific colorectal screening reminder messages based on their perceived category, or “patient segment.”
Values-based communications™
When health-related communications are oriented towards an individual’s value, more patients “get” why the information is relevant to them. Personalizing the content and messaging means that the message makes sense to the patient. This is the concept of values-based communications used by MDH and ARC to encourage patients to get their colon cancer screening and oft-avoided preventive health screening.
Patient segmentation
The connected era we live in has revealed more about people’s healthcare preferences. Cognitive research models can now be applied to healthcare to better understand and incorporate patients’ preferences, so we can assist them in improving the quality of care.
The outcome of this connectedness is to improve our insights into patients’ health status, preferences, and priorities. We are gaining a better understanding of what works and what doesn’t when it comes to sustaining health improvement initiatives.
The Five Health Personalities
Based on proprietary research developed by PatientBond, MDH guided us on their values-based profiling capabilities to place individuals into five “health personality segments,” listed here from the most proactive to the most reactive:
- Self-achievers – “I take ownership of my health and I actively take steps to be healthy. I focus on achieving my goals and objectives. An illness is just another challenge to be overcome.”
- Balance seekers – “I am open to many ideas and options, as long as they make sense for me. I need context to understand ideas and recommendations.”
- Priority jugglers – “I worry more about my family’s health than my own. I am constantly on the go, juggling many responsibilities, so getting sick is not an option.”
- Direction takers – “I look to my physician and other healthcare providers for guidance and direction on what I need to do to take care of my health.”
- Willful endurers – “There are more important things in my life to focus on than improving my health. I live in the “here and now,” and I can handle whatever comes at me.”
Orienting on values means everyone gains a better understanding of how patients see the world. This means content and communications can be “transmitted on the frequency patients are already listening for,” by having a better grasp of “what people hear” as they engage with portals, programs, physicians, and nurses.
Looking for the “a-ha” moment
Using the right words may seem like a simple thing, but it’s remarkably effective when those words are found. When receiving messages geared toward their perceived segment, patients report more “a-ha” moments about things that have too often been confusing or mundane in the past; their health decisions become more precise and appropriate for them.
ARC’s goal was to determine if customized messages for specific patient segments would increase colon cancer screening rates compared to using a single message to all patients.
Response rate
ARC’s goal was to determine if customized messages for specific patient segments would increase colon cancer screening rates compared to using a single message to all patients. There were a total of 5,724 patients that were part of the study. One thousand six hundred twenty-nine patients received messages personalized for them and a control group of 1,662 of the patients received the same messaging that went out each year. The remaining patients received regular reminders but no additional communications.
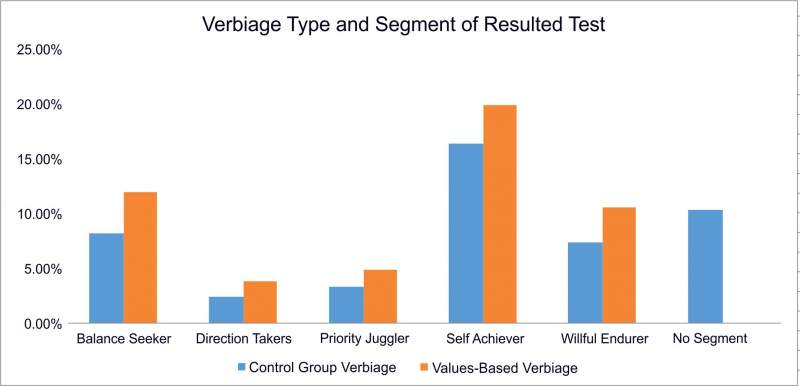
When measuring the response rate per health personality segment, the patients in all segments who received the letters or emails with customized verbiage consistently responded at a higher rate than the control group. Overall, ARC increased email response rates from 27% to 39% and test completion rates increased 2% -5% depending on the segment, as demonstrated below.
In conclusion
Engaging patients in their health and improving health outcomes is a continuous goal of population health. By better understanding how patients prefer to receive guidance – instead of just using a traditional, one-size-fits-all approach – we recognized and aligned with what our patients ultimately wanted to know: ‘Is this screening really relevant to me? And do I really need to do it now?’
Ultimately we confirmed that by using data and an understanding of human psychology, patients were more likely to respond to outreach efforts and make decisions about their health that could ultimately lead to living a longer and higher quality of life.



