Reducing Barriers Related to Telehealth Utilization
By Melissa Fox, MHA, FACMPE, FACHE, COO, Acenda
Telehealth as a method of service delivery has risen in utilization over the past year. However, since this care option is not easily accessible, health care providers must incorporate strategies that ensure underserved populations get equitable access to virtual care.
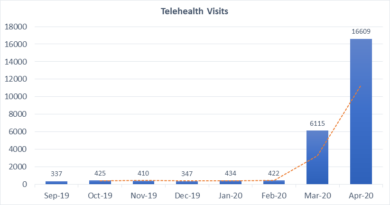
Telehealth is by no means a new approach, but the exponential rise in usage due to COVID-19 has highlighted critical challenges related to reimbursement, privacy, and most importantly, patient access. Restrictions related to telemedicine have been adjusted or relaxed to support in-home delivery of care and potentially reduce the transmission of the coronavirus. This approach is relatively low-risk and high-value since multiple studies have demonstrated that telehealth outcomes are comparable to in-person care and an adequate substitution for face-to-face appointments.
While telehealth services have expanded significantly, many communities do not have adequate technology to complete their care successfully. Whether it is a lack of hardware, limited availability of broadband, or simply being uncomfortable with technology, many people are not able to access telehealth care–even during a raging pandemic.
Unfortunately, these are the same communities that also tend to be the most at risk of chronic health disparities or unnecessary hospital admissions. A 2017 Kaiser Family Foundation study found that 25% of non-elderly adults with Medicaid did not use the internet and 40% did not use email. Additionally, a Harvard study revealed that 21% of rural Americans reported difficulty accessing high-speed internet.
Researchers used data from Mount Sinai to further investigate the healthcare gaps exacerbated by the COVID-19 crisis. Of the 40,000 patients studied between March-May 2020, three main disparities were revealed: race, age, and language preference. Those who identified as White, Asian, or “other/unknown” were more likely to use telehealth services than Black and Hispanic patients. In fact, 60% of Black patients and 48% of Hispanic patients visited the ER during the height of the pandemic rather than using telehealth. Only 24% of adults over 65 used telehealth compared to 47% of adults ages 30 to 49, and only 25% of Spanish-speaking patients utilized telehealth.
This data underscores the inequity of telehealth access and usage, which means health care organizations (HCO) must bridge the care gap by incorporating processes to expand utilization. The following considerations are recommended as part of any telehealth strategy:
- Analyze: Review your current patient data to determine what percentage may be at risk of limited access. This information can be collected by analyzing existing patient demographic data as well as the results of targeted community-based individual surveys. The results can help guide the HCO’s telehealth approach and inform future educational outreach programs. By preparing for the level of need prior to implementation, HCO’s can reduce unnecessary inefficiencies and ensure patients receive the care they need.
- Affiliate: HCO’s may consider partnering with other organizations to support patient access to necessary hardware such as laptops, smartphones, etc., as well as broadband internet. There are federal programs that provide cell phones at no cost to qualifying individuals. Programs such as the Federal Communications Commission’s Rural Health Care Program can serve as a template to replicate for other underrepresented populations experiencing connectivity issues.
- Assess: Continually monitor both telehealth utilization as well as access, and adjust care approaches as needed. This step may involve additional outreach, but may be well worth the effort, so vulnerable patients are not unnecessarily at-risk.
COVID-19 has reinforced the fact that telehealth is an important care option. Supporting equitable access should therefore be a critical strategic consideration to ensure maximum utilization.