Health Care Transformation is More Than Virtual Visits
By Lana Adzhigirey, System Director of Virtual Health, CommonSpirit Health
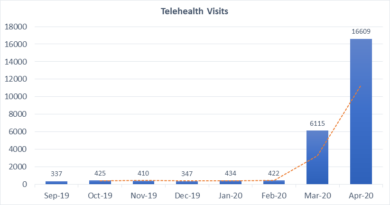
Gone are the days when addressing only the clinical needs of the patients is considered good care. Healthcare systems are facing quickly developing consumer and patient expectations resulting from exposure to convenience and accessibility to services traditionally only offered through brick-and-mortar facilities. Virtual visits have surged during the Covid-19 pandemic as a safe alternative to help curb the spread of infection. As the quarantines lifted, however, patients began returning to in-person care, but the precedent of virtual health has been established.
The Covid-19 Healthcare Coalition Telehealth Impact Study surveyed over 2,000 patients in 2020-2021 and analyzed responses to better understand patient preference around telehealth practices. The authors conclude that most patients indicated that they would have chosen virtual care over an in-person visit or found either modality of the visit (in-person or virtual) acceptable. Given these trends, virtual healthcare is here to stay and patients, providers, healthcare systems, payers, and legislature must continue creating structures to enable high-quality technology-enabled care.
Healthcare organizations are now faced with an enormous opportunity to continue growing the technology-enabled care space which reaches far beyond ambulatory virtual visits. If this transformation is to become sustainable, it must be multifaceted and occur in at least the following three areas: how we collectively define virtual health, how we measure the value of virtual health, and how organization change around virtual care is organized and operationalized.
Transform the definition of virtual care:
The first place of transformation is the definition of virtual care. For a long time, virtual health has been synonymous with “virtual visits” that take place between patients and clinicians via communications technology and frequently interchangeable with the terms “telehealth” and “telemedicine.” The American Telemedicine Association defines telemedicine, also referred to as telehealth or e-medicine, as “the remote delivery of healthcare services, including exams and consultations, over the telecommunications infrastructure.” In light of this rapidly expanding industry, the ATA has expanded the definition to “Technology-Enabled Modalities” and now includes patient education, data transmission, interpretation and analysis, algorithm-enabled diagnostic support, and digital therapeutics, which may include wearables alone or with disease prevention and management.
Additionally, virtual health or virtual care has expanded across the care continuum to include virtual specialist consultations as well as transformational hub and spoke care delivery models such as Virtual nursing, Virtual Companion services, and centralized cardiac monitoring, to name a few. The American Medical Association (AMA) makes a case for the most comprehensive, modern definition of “Digitally Enabled Care,” a fully integrated in-person and virtual care model that hybridize care delivery based on clinical appropriateness and other factors such as convenience and cost. Systems could potentially focus on connecting providers and patients via technology and do it well. Yet to truly appreciate the power of human connectedness, it is necessary to consider the entire care continuum where technology is fully integrated and works seamlessly to enable efficient, evidence-based care which supports care teams rather than caregiver individuals alone.
Transform how the value of virtual care is measured
It is no longer enough to make value decisions based on reimbursement alone as the industry keeps shifting to value-based care. Legislation for virtual health reimbursement is making great strides as states and federal agencies slowly adopt more comprehensive coverage of virtual health services. However, when the dollar for dollar equation is not adding up to care for patients virtually, the true value must be weighed from the perspective of long-term benefits, access, experience, and health equity.
The American Medical Association (AMA) released a report titled Return on Health: Moving Beyond Dollars and Cents in Realizing the Value of Virtual Care. The authors of the report propose a comprehensive framework for measuring the value of digitally enabled care organized in a matrix of environmental variables and virtual care value streams. The five environmental variables are: type of practice, payment arrangement, social determinants of health of the patient populations, clinical use case, and virtual care modality. The five value streams include clinical outcomes, quality and safety, access to care, patient, family and caregiver experience, clinician experience, and financial and operations impact with the overarching health equity impact.
When patients are empowered to access the care they need when they need it and websites are easy to navigate, with nurses readily available to help triage for the most appropriate disposition. When seamless access to vital care teams are available during their hospitalizations, not only the patient wins, but medical costs across the board will begin to decrease as unnecessary ED visits are avoided and acute care length of stay drops.
Clinical, technical, operational, strategy, analytics, and other key teams must drive change as equal partners with shared goals and priorities.
Transform traditional discipline-based teams
Traditional divisions such as IT, nursing and medicine as well as disease-specific service lines must transform to work in cross-functional teams as they work towards shared goals which are unequivocally patient and family-centered. For example, Critical Care clinicians have demonstrated the impact of cross-functional or interdisciplinary teams by transforming intensive care delivery with daily team rounds. Multiple studies have led to these daily interdisciplinary rounds becoming the standard of care for ICU patients worldwide. Additionally, when methodology such as Lean Six Sigma or the like is applied, the results can be even more impressive. Trzeciak et all (2018) studied 259 ICU patient cases before and after the redesign of the rounds using Lean methodology and reported significant decreases in median hospital length of stay (24% decrease, p < .001) and median hospital direct cost per case dropped accordingly by 27% ($66,335 vs. $48,370, p < .001).
When traditionally clinical-focused teams are driving change independent of other teams and vice versa, the lack of shared focus and shared priorities often leads to silos and transformative programs stall. Infrastructure may be built for EHR but inadequate for bidirectional video streaming. Support is frequently an afterthought and falls on clinicians who are already overwhelmed with high workloads and clinical care. Clinicians are fearful that decisions impacting them will be made without their input which creates an environment of control rather than collaboration and collegiality. Clinical, technical, operational, strategy, analytics, and other key teams must drive change as equal partners with shared goals and priorities.
In summary, healthcare is at the precipice of some of the most significant transformation opportunities. But in order for Virtual care or technology-enabled care to succeed and drive better patient outcomes across the care continuum and to contribute to health equity improvements, transformations must take place in how virtual care is defined, how the value is measured, and how organizational change is delivered by cross-functional teams as equal partners in care.