Remote Patient Monitoring: Transforming Care Delivery in the New Digital Era
By Nasim Rezanejad, MD, MS; Adjunct Professor in Health Informatics, University of St. Thomas-Houston
The term “Remote Patient Monitoring” or RPM refers to the use of digital technologies to collect and relay patients’ data to healthcare professionals. The remote patient monitoring field has grown over the last decade and is at a turning point with enormous opportunities to improve health outcomes, improve patient experience and increase affordability.
Simple technologies can connect patients and doctors in a much more intimate way, where the doctors know what is going on without patients coming to a clinic and disrupting their lives every couple of days or becoming inpatients. RPM has the potential to transform disease management; especially for patients with chronic conditions. It can expand healthcare access to underserved populations, including those facing mobility challenges and rural residents.
RPM has been underutilized, and it would be ideal to target it to patients with severe illnesses or higher-risk situations. It can be used for patients who are doing well with their chronic illness and might do well for longer with remote monitoring. Unfortunately, at this point, access to RPM is often based on where a person lives and who their provider is rather than which patients stand to clinically benefit. There are certain patients out there who are going to really benefit from using these technologies.
It is a fundamental shift for providers to determine who will benefit more from using these technologies.
There are two main categories of Remote Patient Monitoring:
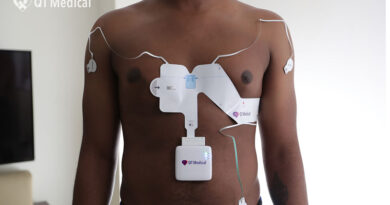
Remote Physiologic Monitoring: Devices that collect physiologic data from the body like blood pressure cuffs, weighing scales, and pulse oximeters- These are devices that gather and monitor the data. The patient does not need to be involved in moving that data. They are transmitted through Bluetooth or to the EHR and the provider gets them.
Remote Therapeutic Monitoring: Much more based on software- Remote Physical Therapy, Respiratory, and Cognitive Behavioral Therapy.
In a quest to improve and establish RPM, we are faced with a few limitations for both clinicians and patients:
1. Technological limitations: How hard is it to get information from the machine in the patient’s house to the doctor’s hands?
2. Clinical limitations: Do we have patients that will have access to receive correct type of care via technology and have the best practices of what to do with the information?
3. Financing system limitations: What supports both sides so that the patients can send that information, the physicians can monitor and act on that and be reimbursed for the time.
4. User technological limitations: Relations with technology, trust in technology, familiarity, how they interact on an individual or community level, and how to engage equally, so everyone knows they have a fair shot of using this life-changing technology.
5. Reimbursement limitations: Billing is still important for keeping the operations running- Figure out how to deploy it and make it work for everyone. Although, billing should not be an obstacle, as clinicians need to deliver care!
6. Data limitations: Clinicians and policymakers need data to address issues around clinicians’ burnout- to help make sure that clinicians can spend the time they need to have one-on-one with the patients who need more time one-on-one and with the technology that is useful. So, there is an incredible value in data collection and studies.
For payers and providers, it is essential to optimize the use of these emerging technologies across three major categories:
1. Service coverage- Clear clinical guidelines on who should use these services and for how long, more flexible billing options for medical providers and an expansion of remote therapeutic monitoring codes to include a broader range of conditions.
2. Ensuring high quality and equitable use of remote monitoring services- Policies to enhance access for underserved populations.
3. Patient privacy and security- Communicate whether there are gaps in privacy procedures. Besides HIPPA, cybersecurity is foundational to medical device safety and effectiveness, and it goes beyond privacy and healthcare in the context of these technologies.
Furthermore, there should be some guidelines in place for each of the devices. The guidelines are set by the FDA’s definition of a medical device, and the FDA evaluates them to see if they do what they are supposed to do. However, this does not mean that they are being used the right way. Guidelines can right size the use of these tools, making sure the people who need the technology have access to it at the right time and at the right place. Since the practice of medicine is completely outside of FDA’s purview, medical societies can work with federal agencies to get guidelines. This is not prescriptive, so it will provide guidelines that will allow medical providers to do more of what they should be doing. Without these guidelines, we end up underutilizing these services and patient care or over-utilizing them, leading to unnecessary spending.
To optimize the use of these technologies, policymakers should take steps to build off evidence and optimally target the use of these services. It is a fundamental shift for providers to determine who will benefit more from using these technologies.
The clinicians can use clinical guidelines and make simple attestations indicating why they use technology. In addition, simple checks can target that kind of technology to sample the patients who will benefit most.
In conclusion, making sure that policy follows science is the one action that needs to be taken; in order to use each of the devices needed for remote patient monitoring.